I am a gastroenterologist. This is a blog of the ERCPs and related endoscopic procedures carried out at my department. Dr Adnan Salim.
Saturday, April 26, 2014
Migrated biliary stent
Friday, April 25, 2014
Extra large diverticulae flanking ampulla
Lost to follow up
This 45 year old gentleman had suffered from bile duct injury whilst undergoing an open cholecystectomy 10 months ago. The surgeons placed a drain (A: red arrow shows the drain. White arrow shows the large leak-almost looking like the gallbladder in shape. Blue arrow shows the main bile duct). An MRI was done soon after and confirmed the leakage (B: red arrows show the bile leak). He was reffered to our facility and we had placed a 10 French 10cm long plastic stents to bridge the leak. (C: white arrows show the stent) . This was about ten months ago. He was then lost to follow up. He resurfaced at our outpatient out of curiosity asking what was to be done about the Stent we had placed. When questioned as to why he hadn't turned up a month after the procedure, he said he had been told by his physician that his condition has been cured and he needs no more treatment. The moment we went in for ERCP, we were greeted by a normal ampulla with no sign of his placed stent. We thought it had migrated inwards but that wasn't the case as it didn't show up on flouroscopy either. One thing we noted was almost absent bike flow from the ampulla and normal flow from another opening just above it (D: Blue arrow marks the ampulla and white arrow indicates the second opening above it with smeared bile). This second opening was obviously a fistula. Cannulation and contrast injection showed no bile leakage (E: white arrows show the bile duct. Even the fistulous track wasn't outlined). We concluded that the Stent had slipped out and his bole was driving through the fistula. The procedure was ended by a sphincterotomy which was extended to include the fistulous opening above the ampulla (F: white arrow).
Wednesday, April 9, 2014
The brothers diverticulae
Third follow up ERCP for post transplant anastomotic biliary stricture (CASE C)
Wednesday, April 2, 2014
Clearing the pancreatic duct
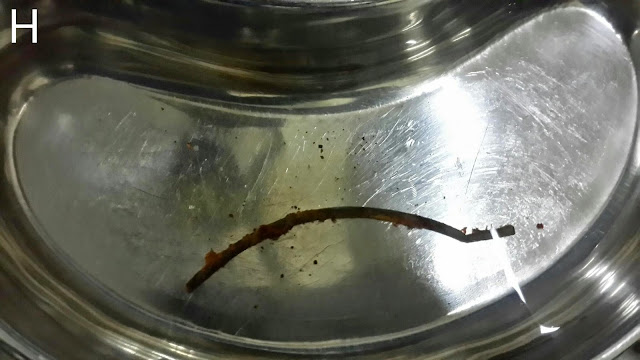
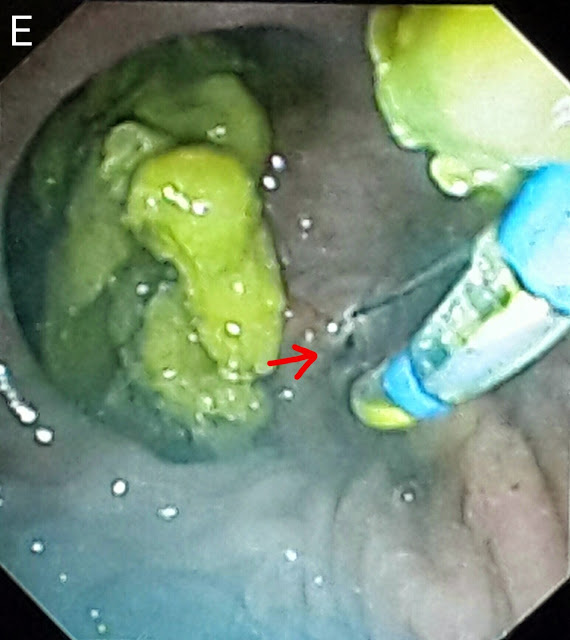
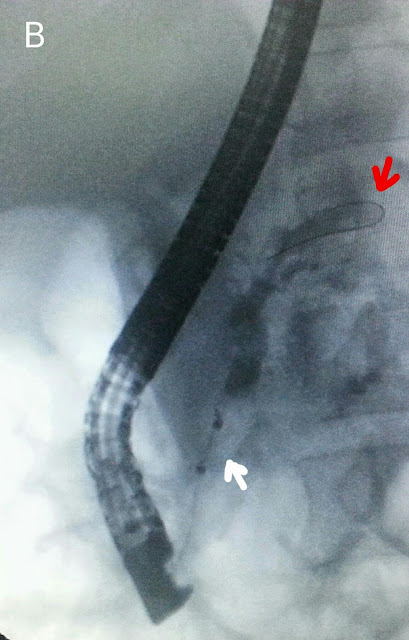
This 30 year old gentleman had developed biliary pancreatitis. He was treated at another facility a month ago where a papillotomy was done and his CBD was cleared of stones/sludge. A straight 10 French stent of 5 cm length was passed. The pancreatic duct could not be cleared at that time as duct access was unsuccessful. The patient was then referred to us. We were greeted with a post-papillotomy papillary with sign of the previous stent-it must have slipped keeping in mind the papillotomy (perhaps a pigtail stent shoulder been used). We were lucky in gaining rapid pancreatic duct access and congrats injection clearly showed two negative shadows (A: white arrows). The guidewire was then advanced further (B: red arrow) and a balloon assembly was then pushed over it (B: white arrow). The pancreatic duct was the swept with the balloon (C: white arrow shows the inflated balloon in the middle of the pancreatic duct). A lot of small white stones and sludge was removed by multiple balloon sweeps (D1 & D2: red arrows). An occlusion pancreaticogram with the balloon inflated at the distal end of the pancreatic duct (E: white arrow) showed a clear duct with no stones.
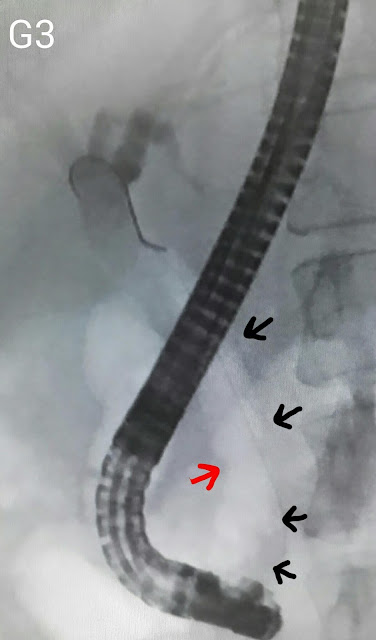
We then accessed the CBD (F: blue arrow shows the papillotome in the CBD. White arrow marks the opening of the pancreatic duct in the papilla). Contrast injection outlined a clear bile duct (G: red arrows show the bile duct. White arrows show the contrast in the pancreatic duct). The CBD was swept with balloon.
Second (actually 3rd) ERCP for post transplant biliary leak
This 60 year old gentleman had earlier undergone ERCP and stenting for an anastomotic biliary leakage a few months earlier http://ercp365.bl...

-
This patient was a 20 year old gentleman who had suffered blunt abdominal trauma during motorcycle accident. He developed a pancreatic absce...
-
This 60 year old gentleman had earlier undergone ERCP and stenting for an anastomotic biliary leakage a few months earlier http://ercp365.bl...
-
This 70 year old gentleman had previously undergone placement of a metallic biliary stent last year for an ampullary tumor. He was subseque...