This gentleman had recently undergone a live related liver transplant. His bilirubin levels started to rise along with his alkaline phosphatase. An anastomotic stricture was suspected and confirmed on MRCP (A: red arrow shows the strictured area along the left maim duct). A guidewire was passed into the left system (B: black arrows mark the guidewire in the left ductal system). A TTS stricture dilatation balloon was manoeuvred across the affected segment and inflated to 9mm (C: black arrows indicate the balloon in the stricture site. The balloon isn't clearly visible because we haven't mixed any contrast with the saline). Repeat contrast injection some improvement in ductal filling (D). We then placed a plastic stent of 10 French diameter and 12 cm length (E: black arrows mark the deployed stent).
I am a gastroenterologist. This is a blog of the ERCPs and related endoscopic procedures carried out at my department. Dr Adnan Salim.
Wednesday, February 25, 2015
Fourth follow-up ERCP for post lover transplant anastomotic stricture (CASE A)
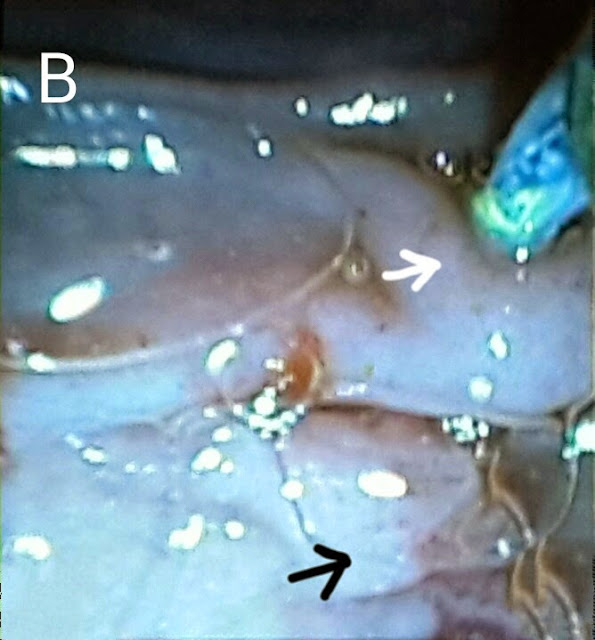
This 50 year old gentleman had come for his 4th follow up procedure after developing jaundice and recurrent fever. We removed his old plastic sent placed during his previous (3rd) ERCP http://ercp365.blogspot.com/2014/09/third-follow-up-ercp-for-post.html using a snare. Contrast injection outlined the anastomotic stricture (A: black arrow). We dilated the stricture using a TTS balloon inflated to 8mm (B: white arrows show the balloon assembly in place at the stricture site with the balloon inflated). A 10 French plastic stent of 12 cm length was placed.
Tuesday, February 3, 2015
To boldly drain what others have not drained before
This 26 year old lady had a history of recurrent cholangitis. She had extra hepatic portal venous obstruction with varies at her porta causing compression of the extra hepatic biliary channels. She had previously undergone three ERCPs. The second ERCP showed her dilated left and right biliary systems (A: black arrows) with luminal narrowing of the confluence, CHD & CBD (A: white arrows). Following dilatation with a graduated dilatation catheter, a 10 French plastic stent had been placed in her right system (B: black arrows) but her left system could not be cannulated (B: white arrows). On her 3rd ERCP, the stent had been removed. Now, 4 months later, she presented with cholangitis. Her MRCP images showed the same findings along with stones on the CBD (C: red arrow marks the calculi, black arrows show the narrow CBD, white arrow indicates the narrowing at the hilum and blue arrows show the dilated right and left ductal systems). We booked her for her 4th ERCP. Our guidewire was first manoeuvred into her left system (D: black arrow shows the guidewire and white arrow shows the dilated left system). This was followed by dilatation of the track using a 10 French graduated dilatation catheter (E: white arrows show the dilatation catheter). We then swept the CBD with a biliary balloon (F:black arrows mark the balloon assembly in the CBD) and a moderate amount of small calculi and sludge was removed (G1: red arrows mark the removed calculi. G2: black arrow shows the "clean sweep" ampulla). We then passed another guidewire in the right system (H: black and white arrows show the two guide wires in the right and left systems, respectively). A 10 French plastic stent of 12 cm length was passed into the right system (I: black arrows mark the stent in the right main duct). A thinner 7 French stent (also of 12 cm length) was then passed into the left system (J: white arrows show the stent in the left main duct while black arrows show the first stent in the right system. K: red arrows show the two stents draining happily in the duodenal lumen).
Monday, February 2, 2015
Unexpected: Doing ERCP on a patient we had referred for surgery many months ago
This 13 year old girl was first seen by us over a year ago in June last year (The case was posted on the blog in August) http://ercp365.blogspot.com/2013/08/pancreatic-duct-calculi.html. She had been having recurrent episodes of pancreatitis. Her ERCP showed multiple pancreatic duct stones (A: white arrows) and a diagnosis of pancreatic divisum as the cause of pancreatitis was made. At that time, looking at the number of stones in the pancreatic duct, we had referred this patient for surgery. The patient's family seemed reluctant for any surgery however and turned up at our outpatient again after over a year in which she had undergone an ERCP at another centre as well (No attempts were made at stone extraction in that attempt either). We again tried to convince the family for surgery but they didn't seem willing. She was put on list again and this time around we went in first via the accessory papilla (B: white arrow indicates the accessory papilla and black arrow marks the major papilla). Contrast injection outlined a grossly dilated pancreatic duct without any negative shadows (C: black arrows show the pancreatic duct). We did a wide papillotomy at the accessory papilla (D). The inner tissue was obviously not what we normally see and showed the degree of fibrosis secondary to chronic repeated inflammation (E: black arrow). A stone extraction balloon assembly was manoeuvred into the pancreatic duct (F: black arrow). The pancreatic duct was swept with the balloon (G: white arrow), which didn't result in extrusion of any debris. This was followed by an occlusion pancreaticogram (H: white arrow shows the inflated balloon and black arrows show a clear dilated pancreatic duct free of stones). The guidewire was withdrawn and then reinserted, this time via the major papilla and into the common bile duct (I: black arrows). We ended the procedure with a cholangiogram which outlined a clear CBD (J: black arrows). Retrospectively, it is possible that the stones seen the first time around in the pancreatic duct were actually aggregations of debris and this had cleared over the past year. In any case we hope she fares well and is able to avoid surgery.
Subscribe to:
Posts (Atom)
Second (actually 3rd) ERCP for post transplant biliary leak
This 60 year old gentleman had earlier undergone ERCP and stenting for an anastomotic biliary leakage a few months earlier http://ercp365.bl...

-
This patient was a 20 year old gentleman who had suffered blunt abdominal trauma during motorcycle accident. He developed a pancreatic absce...
-
This 60 year old gentleman had earlier undergone ERCP and stenting for an anastomotic biliary leakage a few months earlier http://ercp365.bl...
-
This 70 year old gentleman had previously undergone placement of a metallic biliary stent last year for an ampullary tumor. He was subseque...